
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Pathophysiology
- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes
- Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Nan Hee Kim
- Diabetes Metab J. 2024;48(1):37-52. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0193
- 2,183 View
- 219 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
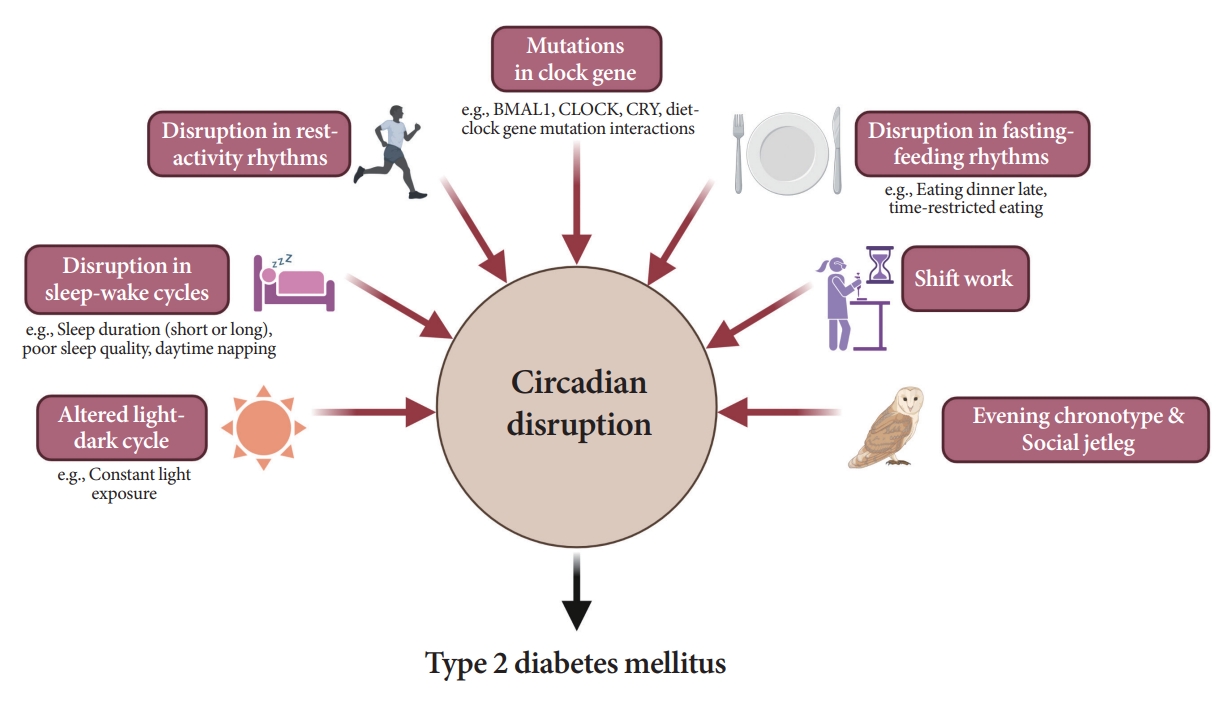
ePub - Novel strategies are required to reduce the risk of developing diabetes and/or clinical outcomes and complications of diabetes. In this regard, the role of the circadian system may be a potential candidate for the prevention of diabetes. We reviewed evidence from animal, clinical, and epidemiological studies linking the circadian system to various aspects of the pathophysiology and clinical outcomes of diabetes. The circadian clock governs genetic, metabolic, hormonal, and behavioral signals in anticipation of cyclic 24-hour events through interactions between a “central clock” in the suprachiasmatic nucleus and “peripheral clocks” in the whole body. Currently, circadian rhythmicity in humans can be subjectively or objectively assessed by measuring melatonin and glucocorticoid levels, core body temperature, peripheral blood, oral mucosa, hair follicles, rest-activity cycles, sleep diaries, and circadian chronotypes. In this review, we summarized various circadian misalignments, such as altered light-dark, sleep-wake, rest-activity, fasting-feeding, shift work, evening chronotype, and social jetlag, as well as mutations in clock genes that could contribute to the development of diabetes and poor glycemic status in patients with diabetes. Targeting critical components of the circadian system could deliver potential candidates for the treatment and prevention of type 2 diabetes mellitus in the future.
- Technology/Device
- Clinical and Lifestyle Determinants of Continuous Glucose Monitoring Metrics in Insulin-Treated Patients with Type 2 Diabetes Mellitus
- Da Young Lee, Namho Kim, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Jihee Kim, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Sung-Min Park, Nan Hee Kim
- Diabetes Metab J. 2023;47(6):826-836. Published online August 24, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0273

- 1,800 View
- 191 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There was limited evidence to evaluate the association between lifestyle habits and continuous glucose monitoring (CGM) metrics. Thus, we aimed to depict the behavioral and metabolic determinants of CGM metrics in insulin-treated patients with type 2 diabetes mellitus (T2DM).
Methods
This is a prospective observational study. We analyzed data from 122 insulin-treated patients with T2DM. Participants wore Dexcom G6 and Fitbit, and diet information was identified for 10 days. Multivariate-adjusted logistic regression analysis was performed for the simultaneous achievement of CGM-based targets, defined by the percentage of time in terms of hyper, hypoglycemia and glycemic variability (GV). Intake of macronutrients and fiber, step counts, sleep, postprandial C-peptide-to-glucose ratio (PCGR), information about glucose lowering medications and metabolic factors were added to the analyses. Additionally, we evaluated the impact of the distribution of energy and macronutrient during a day, and snack consumption on CGM metrics.
Results
Logistic regression analysis revealed that female, participants with high PCGR, low glycosylated hemoglobin (HbA1c) and daytime step count had a higher probability of achieving all targets based on CGM (odds ratios [95% confidence intervals] which were 0.24 [0.09 to 0.65], 1.34 [1.03 to 1.25], 0.95 [0.9 to 0.99], and 1.15 [1.03 to 1.29], respectively). And participants who ate snacks showed a shorter period of hyperglycemia and less GV compared to those without.
Conclusion
We confirmed that residual insulin secretion, daytime step count, HbA1c, and women were the most relevant determinants of adequate glycemic control in insulin-treated patients with T2DM. In addition, individuals with snack consumption were exposed to lower times of hyperglycemia and GV. -
Citations
Citations to this article as recorded by- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
Lotte Bogaert, Iris Willems, Patrick Calders, Eveline Dirinck, Manon Kinaupenne, Marga Decraene, Bruno Lapauw, Boyd Strumane, Margot Van Daele, Vera Verbestel, Marieke De Craemer
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2024; 18(4): 102995. CrossRef
- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
- Association of Body Mass Index and Fracture Risk Varied by Affected Bones in Patients with Diabetes: A Nationwide Cohort Study (Diabetes Metab J 2023;47:242-54)
- So Young Park
- Diabetes Metab J. 2023;47(3):437-438. Published online May 26, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0100
- [Original]
- 1,046 View
- 60 Download
- Others
- Fasting Glucose Variability and the Risk of Dementia in Individuals with Diabetes: A Nationwide Cohort Study
- Da Young Lee, Jaeyoung Kim, Sanghyun Park, So Young Park, Ji Hee Yu, Ji A Seo, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Kyungdo Han, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):923-935. Published online May 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0346
- 5,617 View
- 254 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated whether fasting glucose (FG) variability could predict the risk of dementia.
Methods
This cohort study analyzed data from Koreans with diabetes after at least three health examinations by the Korean National Health Insurance Corporation between 2005 and 2010, which included at least one examination between 2009 and 2010. A total of 769,554 individuals were included, excluding those aged <40 years and those with dementia. FG variability was measured using the variability independent of the mean (FG-VIM). The incidence of dementia was defined by the International Classification of Diseases 10th Revision codes and prescription of anti-dementia medication and was subdivided into Alzheimer’s disease (AD) and vascular dementia (VD).
Results
During the 6.9-year follow-up, 54,837, 41,032, and 6,892 cases of all-cause dementia, AD, and VD, respectively, were identified. Cox proportional regression analyses showed that as the FG-VIM quartile increased, the risk of dementia serially increased after adjustment for metabolic factors, income status, and diabetes-related characteristics, including the mean FG. Participants in FG-VIM quartile 4 showed a 18%, 19%, and 17% higher risk for all-cause dementia, AD, and VD, respectively, than those in quartile 1; this particularly included non-obese patients with a longer duration of diabetes, high FG levels, dyslipidemia, and those taking glucose-lowering medications. Conversely, the baseline FG status and dementia showed a U-shaped association.
Conclusion
Increased FG variability over 5 years can predict the risk of dementia in individuals with diabetes in Korea. This finding was more pronounced in patients with less favorable metabolic profiles. -
Citations
Citations to this article as recorded by- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
Sung Hoon Kang, Yunjin Choi, Su Jin Chung, Seok-Joo Moon, Chi Kyung Kim, Ji Hyun Kim, Kyungmi Oh, Joon Shik Yoon, Sang Won Seo, Geum Joon Cho, Seong-Beom Koh
Frontiers in Aging Neuroscience.2024;[Epub] CrossRef - Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
Vishal Chavda, Dhananjay Yadav, Snehal Patel, Minseok Song
Brain Sciences.2024; 14(3): 284. CrossRef - The Association of Glucose Variability and Dementia Incidence in Latinx Adults with Type 2 Diabetes: A Retrospective Study
Heather Cuevas, Elizabeth Muñoz, Divya Nagireddy, Jeeyeon Kim, Grace Ganucheau, Fathia Alomoush
Clinical Nursing Research.2023; 32(2): 249. CrossRef - The effects of long-term cumulative HbA1c exposure on the development and onset time of dementia in the patients with type 2 diabetes mellitus: Hospital based retrospective study (2005–2021)
Sunyoung Cho, Choon Ok Kim, Bong-soo Cha, Eosu Kim, Chung Mo Nam, Min-Gul Kim, Min Soo Park
Diabetes Research and Clinical Practice.2023; 201: 110721. CrossRef - Physiological Mechanisms Inherent to Diabetes Involved in the Development of Dementia: Alzheimer’s Disease
Himan Mohamed-Mohamed, Victoria García-Morales, Encarnación María Sánchez Lara, Anabel González-Acedo, Teresa Pardo-Moreno, María Isabel Tovar-Gálvez, Lucía Melguizo-Rodríguez, Juan José Ramos-Rodríguez
Neurology International.2023; 15(4): 1253. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef
- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
- Technology/Device
- Comparison of Laser and Conventional Lancing Devices for Blood Glucose Measurement Conformance and Patient Satisfaction in Diabetes Mellitus
- Jung A Kim, Min Jeong Park, Eyun Song, Eun Roh, So Young Park, Da Young Lee, Jaeyoung Kim, Ji Hee Yu, Ji A Seo, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):936-940. Published online March 30, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0293
- 5,277 View
- 256 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Self-monitoring of capillary blood glucose is important for controlling diabetes. Recently, a laser lancing device (LMT-1000) that can collect capillary blood without skin puncture was developed. We enrolled 150 patients with type 1 or 2 diabetes mellitus. Blood sampling was performed on the same finger on each hand using the LMT-1000 or a conventional lancet. The primary outcome was correlation between glucose values using the LMT-1000 and that using a lancet. And we compared the pain and satisfaction of the procedures. The capillary blood sampling success rates with the LMT-1000 and lancet were 99.3% and 100%, respectively. There was a positive correlation (r=0.974, P<0.001) between mean blood glucose levels in the LMT-1000 (175.8±63.0 mg/dL) and conventional lancet samples (172.5±63.6 mg/dL). LMT-1000 reduced puncture pain by 75.0% and increased satisfaction by 80.0% compared to a lancet. We demonstrated considerable consistency in blood glucose measurements between samples from the LMT-1000 and a lancet, but improved satisfaction and clinically significant pain reduction were observed with the LMT-1000 compared to those with a lancet.
-
Citations
Citations to this article as recorded by- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
Chul Kyu Yun, Eui Kyung Choi, Hyung Jin Kim, Jaeyoung Kim, Byung Cheol Park, Kyuhee Park, Byung Min Choi
Journal of Perinatology.2024;[Epub] CrossRef
- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
- Technology/Device
- Assessment of Insulin Secretion and Insulin Resistance in Human
- So Young Park, Jean-François Gautier, Suk Chon
- Diabetes Metab J. 2021;45(5):641-654. Published online September 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0220

- 14,153 View
- 879 Download
- 47 Web of Science
- 23 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
- The impaired insulin secretion and increased insulin resistance (or decreased insulin sensitivity) play a major role in the pathogenesis of all types of diabetes mellitus (DM). It is very important to assess the pancreatic β-cell function and insulin resistance/ sensitivity to determine the type of DM and to plan an optimal management and prevention strategy for DM. So far, various methods and indices have been developed to assess the β-cell function and insulin resistance/sensitivity based on static, dynamic test and calculation of their results. In fact, since the metabolism of glucose and insulin is made through a complex process related with various stimuli in several tissues, it is difficult to fully reflect the real physiology. In order to solve the theoretical and practical difficulties, research on new index is still in progress. Also, it is important to select the appropriate method and index for the purpose of use and clinical situation. This review summarized a variety of traditional methods and indices to evaluate pancreatic β-cell function and insulin resistance/sensitivity and introduced novel indices.
-
Citations
Citations to this article as recorded by- Polyphenol-Rich Extract of Fermented Chili Pepper Alleviates Insulin Resistance in HepG2 Cells via Regulating INSR, PTP1B, PPAR-γ, and AMPK Pathways
Tao Wang, Meiqi Li, Shengbao Cai, Linyan Zhou, Xiaosong Hu, Junjie Yi
Fermentation.2023; 9(2): 84. CrossRef - 2,3-Dihydrosorbicillin and chrysopanol stimulate insulin secretion in INS-1 cells
Dahae Lee, Jaekyung Kim, Sungyoul Choi, Jinwon Choi, Jin Woo Lee, Ki Sung Kang, Sang Hee Shim
Bioorganic & Medicinal Chemistry Letters.2023; 83: 129186. CrossRef - Insulin: A connection between pancreatic β cells and the hypothalamus
Brenda De la Cruz Concepción, Yaccil Adilene Flores Cortez, Martha Isela Barragán Bonilla, Juan Miguel Mendoza Bello, Monica Espinoza Rojo
World Journal of Diabetes.2023; 14(2): 76. CrossRef - The Metabolic Score for Insulin Resistance (METS-IR) Predicts Cardiovascular Disease and Its Subtypes in Patients with Hypertension and Obstructive Sleep Apnea
Wenbo Yang, Xintian Cai, Junli Hu, Wen Wen, Heizhati Mulalibieke, Xiaoguang Yao, Ling Yao, Qing Zhu, Jing Hong, Qin Luo, Shasha Liu, Nanfang Li
Clinical Epidemiology.2023; Volume 15: 177. CrossRef - Association between dietary patterns and biomarkers in connection with diabetes mellitus in adolescents: A systematic review
Bernardo Paz Barboza, Camila Tureck, Liliana Paula Bricarello, Mariane de Almeida Alves, Anabelle Retondario, Amanda de Moura Souza, Ricardo Fernandes, Francisco de Assis Guedes de Vasconcelos
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(4): 685. CrossRef - PNPLA3 rs738409 risk genotype decouples TyG index from HOMA2-IR and intrahepatic lipid content
Ákos Nádasdi, Viktor Gál, Tamás Masszi, Anikó Somogyi, Gábor Firneisz
Cardiovascular Diabetology.2023;[Epub] CrossRef - Ethnic Variability in Glucose and Insulin Response to Rice Among Healthy Overweight Adults: A Randomized Cross-Over Study
Amena Sadiya, Vidya Jakapure, Vijay Kumar
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 993. CrossRef - Familial partial lipodystrophy type 2 and obesity, two adipose tissue pathologies with different inflammatory profiles
Guillaume Treiber, Marie-Paule Gonthier, Alice Guilleux, Samir Medjane, Oriane Bonfanti, Muriel Cogne, Olivier Meilhac, Estelle Nobecourt
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Discriminant Model for Insulin Resistance in Type 2 Diabetic Patients
Erislandis López-Galán, Rafael Barrio-Deler, Manuel Alejandro Fernández-Fernández, Yaquelin Del Toro-Delgado, Isaac Enrique Peñuela-Puente, Miguel Enrique Sánchez-Hechavarría, Mario Eugenio Muñoz-Bustos, Gustavo Alejandro Muñoz-Bustos
Medicina.2023; 59(5): 839. CrossRef - Mechanisms of Oxidative Stress in Metabolic Syndrome
Sepiso K. Masenga, Lombe S. Kabwe, Martin Chakulya, Annet Kirabo
International Journal of Molecular Sciences.2023; 24(9): 7898. CrossRef - Estimated Glucose Disposal Rate Predicts Renal Progression in Type 2 Diabetes Mellitus: A Retrospective Cohort Study
Juan Peng, Aimei Li, Liangqingqing Yin, Qi Yang, Jinting Pan, Bin Yi
Journal of the Endocrine Society.2023;[Epub] CrossRef - Transfer RNA Mutation Associated with Type 2 Diabetes Mellitus
Fanny Rizki Rahmadanthi, Iman Permana Maksum
Biology.2023; 12(6): 871. CrossRef - Honokiol improves endothelial function in type 2 diabetic rats via alleviating oxidative stress and insulin resistance
An He, Huilin Yu, Yu Hu, Huiling Chen, Xiang Li, Jian Shen, Rongjuan Zhuang, Yi Chen, Bryan Richard Sasmita, Minghao Luo, Dingyi Lv
Biochemical and Biophysical Research Communications.2022; 600: 109. CrossRef - Relationship of Vitamin A and Thyroid Function in Individuals With Obesity and After Laparoscopic Sleeve Gastrectomy
Bingwei Ma, Peng Yang, Jingyang Gao, Lei Du, Chunjun Sheng, Taofeek Usman, Xingchun Wang, Shen Qu
Frontiers in Nutrition.2022;[Epub] CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - Acyclovir alleviates insulin resistance via activating PKM1 in diabetic mice
Zhuozhou Hu, Jing Zhou, Liang Han, Xiangxiang Li, Chun Li, Tongyu Wu, Jingjing Liu, Wenyang Zhao, Jia Kang, Xinping Chen
Life Sciences.2022; 304: 120725. CrossRef - Identifying Glucose Metabolism Status in Nondiabetic Japanese Adults Using Machine Learning Model with Simple Questionnaire
Tomoki Uchida, Takeshi Kanamori, Takanori Teramoto, Yuji Nonaka, Hiroki Tanaka, Satoshi Nakamura, Norihito Murayama, Rajesh Kaluri
Computational and Mathematical Methods in Medicine.2022; 2022: 1. CrossRef - Elevated triglyceride-glucose (TyG) index predicts impaired islet β-cell function: A hospital-based cross-sectional study
Zi Chen, Jie Wen
Frontiers in Endocrinology.2022;[Epub] CrossRef - Maternal Glycaemic and Insulinemic Status and Newborn DNA Methylation: Findings in Women With Overweight and Obesity
Marion Lecorguillé, Fionnuala M McAuliffe, Patrick J Twomey, Karien Viljoen, John Mehegan, Cecily C Kelleher, Matthew Suderman, Catherine M Phillips
The Journal of Clinical Endocrinology & Metabolism.2022; 108(1): 85. CrossRef - Acanthosis Nigricans: Pointer of Endocrine Entities
Andreea-Maria Radu, Mara Carsote, Mihai Cristian Dumitrascu, Florica Sandru
Diagnostics.2022; 12(10): 2519. CrossRef - Relationship between Insulin Resistance Risk Scales and Non-Alcoholic Fatty Liver Disease and Liver Fibrosis Scales in 219,477 Spanish Workers
José Ignacio Ramírez-Manent, Emilio Martínez-Almoyna, Carlos López, Carla Busquets-Cortés, Hilda González San Miguel, Ángel Arturo López-González
Metabolites.2022; 12(11): 1093. CrossRef - Investigation of Insulin Secretion in Glucose Tolerance Test by the Intake of Novel Imeglimin (Twymeeg)
Hiroshi BANDO, Hiroko OGAWA, Hirohisa URASAKI, Shinji NAGAHIRO, Hiroko URASAKI, Miwako NAKANISHI, Osami WATANABE
Asploro Journal of Biomedical and Clinical Case Reports.2022; 5(3): 113. CrossRef - Evaluation and Screening of Hypoglycemic Activity of Total Ginsenosides GBE-5 Fraction From Panax Ginseng Berry Based on UHPLC–MS Metabolomics
Heyu Wang, Yu Tong, Anqi Wang, Ying Li, Bofan Lu, Hui Li, Lili Jiao, Wei Wu
Frontiers in Nutrition.2022;[Epub] CrossRef
- Polyphenol-Rich Extract of Fermented Chili Pepper Alleviates Insulin Resistance in HepG2 Cells via Regulating INSR, PTP1B, PPAR-γ, and AMPK Pathways
- Response: Cardio-Ankle Vascular Index as a Surrogate Marker of Early Atherosclerotic Cardiovascular Disease in Koreans with Type 2 Diabetes Mellitus (
Diabetes Metab J 2018;42:285-95) - So Young Park, Suk Chon
- Diabetes Metab J. 2018;42(5):449-450. Published online October 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0206
- 2,961 View
- 41 Download
- Clinical Diabetes and Therapeutics
- Cardio-Ankle Vascular Index as a Surrogate Marker of Early Atherosclerotic Cardiovascular Disease in Koreans with Type 2 Diabetes Mellitus
- So Young Park, Sang Ook Chin, Sang Youl Rhee, Seungjoon Oh, Jeong-Taek Woo, Sung Woon Kim, Suk Chon
- Diabetes Metab J. 2018;42(4):285-295. Published online July 27, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0080
- 4,811 View
- 52 Download
- 18 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Carotid artery intima medial thickness (IMT), brachial-ankle pulse wave velocity (baPWV), and ankle-brachial index (ABI) are commonly used surrogate markers of subclinical atherosclerosis in patients with type 2 diabetes mellitus (T2DM). The cardio-ankle vascular index (CAVI) is a complement to the baPWV, which is affected by blood pressure. However, it is unclear which marker is the most sensitive predictor of atherosclerotic cardiovascular disease (ASCVD).
Methods This was a retrospective non-interventional study that enrolled 219 patients with T2DM. The correlations among IMT, ABI, and CAVI as well as the relationship of these tests to the 10-year ASCVD risk were also analyzed.
Results Among the 219 patients, 39 (17.8%) had ASCVD. In the non-ASCVD group, CAVI correlated significantly with IMT after adjusting for confounding variables, but ABI was not associated with CAVI or IMT. The analyses after dividing the non-ASCVD group into three subgroups according to the CAVI score (<8, ≥8 and <9, and ≥9) demonstrated the significant increase in the mean IMT, 10-year ASCVD risk and number of metabolic syndrome risk factors, and decrease in the mean ABI in the high-CAVI group. A high CAVI was an independent risk factor in the non-ASCVD group for both a high 10-year ASCVD risk (≥7.5%; odds ratio [OR], 2.42;
P <0.001) and atherosclerosis (mean IMT ≥1 mm; OR, 1.53;P =0.007).Conclusion In Korean patients with T2DM without ASCVD, CAVI was the most sensitive of several surrogate markers for the detection of subclinical atherosclerosis.
-
Citations
Citations to this article as recorded by- The effects of severe periodontitis on arterial stiffness using cardio‐ankle vascular index in patients with type 2 diabetes
Gizem Torumtay Cin, Semin Melahat Fenkci, Ismail Doğu Kiliç, Halil Serdar Aslan, Cihan İlyas Sevgican, Hande Şenol
Journal of Periodontal Research.2024; 59(1): 74. CrossRef - Prediction of cardiovascular disease using deep learning algorithms to prevent COVID 19
Malathi S, Arockia Raj Y, Abhishek Kumar, V D Ashok Kumar, Ankit Kumar, Elangovan D, V D Ambeth Kumar, Chitra B, a Abirami
Journal of Experimental & Theoretical Artificial Intelligence.2023; 35(6): 791. CrossRef - Association of cardio-ankle vascular index and future major adverse cardiovascular events in older adults living with HIV
Amaraporn Rerkasem, Arunrat Tangmunkongvorakul, Linda Aurpibul, Patumrat Sripan, Wason Parklak, Sothida Nantakool, Kriengkrai Srithanaviboonchai, Kittipan Rerkasem
AIDS Care.2023; 35(4): 591. CrossRef - Impact of Fasting Blood Glucose Levels on Blood Pressure Parameters among Older Adults with Prediabetes
Thapanee Roengrit, Ruchada Sri-Amad, Nawiya Huipao, Suphawadee Phababpha, Piyapong Prasertsri, Francesco Giallauria
The Scientific World Journal.2023; 2023: 1. CrossRef - A framework of biomarkers for vascular aging: a consensus statement by the Aging Biomarker Consortium
Le Zhang, Jun Guo, Yuehong Liu, Shimin Sun, Baohua Liu, Qi Yang, Jun Tao, Xiao-Li Tian, Jun Pu, Huashan Hong, Miao Wang, Hou-Zao Chen, Jie Ren, Xiaoming Wang, Zhen Liang, Yuan Wang, Kai Huang, Weiqi Zhang, Jing Qu, Zhenyu Ju, Guang-Hui Liu, Gang Pei, Jian
Life Medicine.2023;[Epub] CrossRef - Diastolic Pressure and ACR Are Modifiable Risk Factors of Arterial Stiffness in T2DM Without Cardiovascular Disease
Gateano Leto, Lida Tartaglione, Silverio Rotondi, Marzia Pasquali, Ernesto Maddaloni, Carmen Mignogna, Luca D’Onofrio, Simona Zampetti, Angela Carlone, Maria Luisa Muci, Daniela Mastroluca, Valeria Fassino, Raffaella Buzzetti, Sandro Mazzaferro
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): e3857. CrossRef - Risk assessment indicators and brachial-ankle pulse wave velocity to predict atherosclerotic cardiovascular disease
Hung-Ju Ko, Chuan-Chuan Liu, Po-Jui Hsu, Kuang-Chun Hu, Chung-Lieh Hung, Lo-Yip Yu, Yun-Chieh Huang, Shou-Chuan Shih
Medicine.2022; 101(32): e29609. CrossRef - Prediction of Cardiovascular Disease Using Machine Learning Technique—A Modern Approach
Jung-Hwa Kim, Jin-Woo Jeong
Computers, Materials & Continua.2022; 71(1): 855. CrossRef - Cardio-ankle vascular index represents the best surrogate for 10-year ASCVD risk estimation in patients with primary hypertension
Mustafa Tarik Agac, Süret Ağaç, Muhammed Necati Murat Aksoy, Mehmet Bülent Vatan
Clinical and Experimental Hypertension.2021; 43(4): 349. CrossRef - Relation between fragmented QRS complex and cardio-ankle vascular index in asymptomatic subjects
Ali Rıza Akyüz, Sinan Şahin, Ömer Faruk Çırakoğlu, Selim Kul, Turhan Turan, Hakan Erkan
Clinical and Experimental Hypertension.2021; 43(4): 368. CrossRef - Progress of clinical evaluation for vascular aging in humans
Yumin Qiu, Yuanya Liu, Jun Tao
Journal of Translational Internal Medicine.2021; 9(1): 17. CrossRef - Effects of long-term air pollution exposure on ankle-brachial index and cardio-ankle vascular index: A longitudinal cohort study using data from the Electricity Generating Authority of Thailand study
Kanawat Paoin, Kayo Ueda, Prin Vathesatogkit, Thammasin Ingviya, Suhaimee Buya, Arthit Phosri, Xerxes Tesoro Seposo, Nisakron Thongmung, Teerapat Yingchoncharoen, Akiko Honda, Hirohisa Takano, Piyamitr Sritara
International Journal of Hygiene and Environmental Health.2021; 236: 113790. CrossRef The Relationship Between Glycemic Control and Concomitant Hypertension on Arterial Stiffness in Type II Diabetes
Teonchit Nuamchit, Duangduan Siriwittayawan, Piyanuch Thitiwuthikiat
Vascular Health and Risk Management.2020; Volume 16: 343. CrossRef- Relationship between cardio-ankle vascular index and obstructive coronary artery disease
Divya Birudaraju, Lavanya Cherukuri, April Kinninger, Bhanu T. Chaganti, Pishoy Haroun, Sivakrishna Pidikiti, Suvasini Lakshmanan, Sajad Hamal, Ferdinand Flores, Christopher Dailing, Kashif Shaikh, Sion K. Roy, Matthew J. Budoff
Coronary Artery Disease.2020; 31(6): 550. CrossRef - Association of Kidney Function Tests with a Cardio-Ankle Vascular Index in Community-Dwelling Individuals with a Normal or Mildly Decreased Estimated Glomerular Filtration Rate
Javad Alizargar, Chyi-Huey Bai, Nan-Chen Hsieh, Shu-Fang Vivienne Wu, Shih-Yen Weng, Jia-Ping Wu
Medicina.2019; 55(10): 657. CrossRef - Cardiovascular remodeling in patients with diabetic сardiomyopathy
A. S. Veklich, N. A. Koziolova, P. G. Karavaev
Russian Journal of Cardiology.2019; (11): 42. CrossRef - Short‑term impact of aged garlic extract on endothelial function in diabetes: A randomized, double‑blind, placebo‑controlled trial
Sajad Hamal, Lavanya Cherukuri, Divya Birudaraju, Suguru Matsumoto, April Kinninger, Bhanu Chaganti, Ferdinand Flores, Kashif Shaikh, Sion Roy, Matthew Budoff
Experimental and Therapeutic Medicine.2019;[Epub] CrossRef - Association between Breakfast Frequency and Atherosclerotic Cardiovascular Disease Risk: A Cross-Sectional Study of KNHANES Data, 2014–2016
Hyeon Ji Lee, Jieun Jang, Sang Ah Lee, Dong-Woo Choi, Eun-Cheol Park
International Journal of Environmental Research and Public Health.2019; 16(10): 1853. CrossRef - Response: Cardio-Ankle Vascular Index as a Surrogate Marker of Early Atherosclerotic Cardiovascular Disease in Koreans with Type 2 Diabetes Mellitus (Diabetes Metab J 2018;42:285-95)
So Young Park, Suk Chon
Diabetes & Metabolism Journal.2018; 42(5): 449. CrossRef - Letter: Cardio-Ankle Vascular Index as a Surrogate Marker of Early Atherosclerotic Cardiovascular Disease in Koreans with Type 2 Diabetes Mellitus (Diabetes Metab J 2018;42:285-95)
Dongwon Yi
Diabetes & Metabolism Journal.2018; 42(5): 447. CrossRef
- The effects of severe periodontitis on arterial stiffness using cardio‐ankle vascular index in patients with type 2 diabetes
- Complications
- Glycated Albumin Is a More Useful Glycation Index than HbA1c for Reflecting Renal Tubulopathy in Subjects with Early Diabetic Kidney Disease
- Ji Hye Huh, Minyoung Lee, So Young Park, Jae Hyeon Kim, Byung-Wan Lee
- Diabetes Metab J. 2018;42(3):215-223. Published online May 2, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0091
- 4,419 View
- 52 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate which glycemic parameters better reflect urinary N-acetyl-β-D-glucosaminidase (uNAG) abnormality, a marker for renal tubulopathy, in subjects with type 2 diabetes mellitus (T2DM) subjects with normoalbuminuria and a normal estimated glomerular filtration rate (eGFR).
Methods We classified 1,061 participants with T2DM into two groups according to uNAG level—normal vs. high (>5.8 U/g creatinine)—and measured their biochemical parameters.
Results Subjects with high uNAG level had significantly higher levels of fasting and stimulated glucose, glycated albumin (GA), and glycosylated hemoglobin (HbA1c) and lower levels of homeostasis model assessment of β-cell compared with subjects with normal uNAG level. Multiple linear regression analyses showed that uNAG was significantly associated with GA (standardized β coefficient [β]=0.213,
P =0.016), but not with HbA1c (β=−0.137,P =0.096) or stimulated glucose (β=0.095,P =0.140) after adjusting confounding factors. In receiver operating characteristic analysis, the value of the area under the curve (AUC) for renal tubular injury of GA was significantly higher (AUC=0.634; 95% confidence interval [CI], 0.646 to 0.899) than those for HbA1c (AUC=0.598; 95% CI, 0.553 to 0.640), stimulated glucose (AUC=0.594; 95% CI, 0.552 to 0.636), or fasting glucose (AUC=0.558; 95% CI, 0.515 to 0.600). The optimal GA cutoff point for renal tubular damage was 17.55% (sensitivity 59%, specificity 62%).Conclusion GA is a more useful glycation index than HbA1c for reflecting renal tubulopathy in subjects with T2DM with normoalbuminuria and normal eGFR.
-
Citations
Citations to this article as recorded by- Glucagon-Like Peptide 1 Receptor Agonist Improves Renal Tubular Damage in Mice with Diabetic Kidney Disease
Ran Li, Dunmin She, Zhengqin Ye, Ping Fang, Guannan Zong, Yong Zhao, Kerong Hu, Liya Zhang, Sha Lei, Keqin Zhang, Ying Xue
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 1331. CrossRef - Use of glycated albumin for the identification of diabetes in subjects from northeast China
Guo-Yan Li, Hao-Yu Li, Qiang Li
World Journal of Diabetes.2021; 12(2): 149. CrossRef - Diabetic Kidney Disease, Cardiovascular Disease and Non-Alcoholic Fatty Liver Disease: A New Triumvirate?
Carolina M. Perdomo, Nuria Garcia-Fernandez, Javier Escalada
Journal of Clinical Medicine.2021; 10(9): 2040. CrossRef - Empagliflozin reduces high glucose-induced oxidative stress and miR-21-dependent TRAF3IP2 induction and RECK suppression, and inhibits human renal proximal tubular epithelial cell migration and epithelial-to-mesenchymal transition
Nitin A. Das, Andrea J. Carpenter, Anthony Belenchia, Annayya R. Aroor, Makoto Noda, Ulrich Siebenlist, Bysani Chandrasekar, Vincent G. DeMarco
Cellular Signalling.2020; 68: 109506. CrossRef - Glycated Plasma Proteins as More Sensitive Markers for Glycemic Control in Type 1 Diabetes
Lina Zhang, Qibin Zhang
PROTEOMICS – Clinical Applications.2020;[Epub] CrossRef - Glycated albumin and its variability: Clinical significance, research progress and overall review
Dongjun Dai, Yifei Mo, Jian Zhou
Obesity Medicine.2020; 19: 100256. CrossRef - Hepatic fibrosis is associated with total proteinuria in Korean patients with type 2 diabetes
Eugene Han, Yongin Cho, Kyung-won Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-wan Lee
Medicine.2020; 99(33): e21038. CrossRef - Increasing waist circumference is associated with decreased levels of glycated albumin
Yiting Xu, Xiaojing Ma, Yun Shen, Yufei Wang, Jian Zhou, Yuqian Bao
Clinica Chimica Acta.2019; 495: 118. CrossRef - Glucometabolic characteristics and higher vascular complication risk in Korean patients with type 2 diabetes with non-albumin proteinuria
Yongin Cho, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-wan Lee
Journal of Diabetes and its Complications.2019; 33(8): 585. CrossRef - Association of urinary acidification function with the progression of diabetic kidney disease in patients with type 2 diabetes
Huanhuan Zhu, Xi Liu, Chengning Zhang, Qing Li, Xiaofei An, Simeng Liu, Lin Wu, Bo Zhang, Yanggang Yuan, Changying Xing
Journal of Diabetes and its Complications.2019; 33(11): 107419. CrossRef
- Glucagon-Like Peptide 1 Receptor Agonist Improves Renal Tubular Damage in Mice with Diabetic Kidney Disease
- Obesity and Metabolic Syndrome
- Air Pollution Has a Significant Negative Impact on Intentional Efforts to Lose Weight: A Global Scale Analysis
- Morena Ustulin, So Young Park, Sang Ouk Chin, Suk Chon, Jeong-taek Woo, Sang Youl Rhee
- Diabetes Metab J. 2018;42(4):320-329. Published online April 24, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0104
- 4,270 View
- 40 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Air pollution causes many diseases and deaths. It is important to see how air pollution affects obesity, which is common worldwide. Therefore, we analyzed data from a smartphone application for intentional weight loss, and then we validated them.
Methods Our analysis was structured in two parts. We analyzed data from a cohort registered to a smartphone application in 10 large cities of the world and matched it with the annual pollution values. We validated these results using daily pollution data in United States and matching them with user information. Body mass index (BMI) variation between final and initial login time was considered as outcome in the first part, and daily BMI in the validation. We analyzed: daily calories intake, daily weight, daily physical activity, geographical coordinates, seasons, age, gender. Weather Underground application programming interface provided daily climatic values. Annual and daily values of particulate matter PM10 and PM2.5 were extracted. In the first part of the analysis, we used 2,608 users and then 995 users located in United States.
Results Air pollution was highest in Seoul and lowest in Detroit. Users decreased BMI by 2.14 kg/m2 in average (95% confidence interval, −2.26 to −2.04). From a multilevel model, PM10 (β=0.04,
P =0.002) and PM2.5 (β=0.08,P <0.001) had a significant negative effect on weight loss when collected per year. The results were confirmed with the validation (βAQI*time=1.5×10–5;P <0.001) by mixed effects model.Conclusion This is the first study that shows how air pollution affects intentional weight loss applied on wider area of the world.
-
Citations
Citations to this article as recorded by- What could be the reasons for not losing weight even after following a weight loss program?
Jyoti Dabas, S. Shunmukha Priya, Akshay Alawani, Praveen Budhrani
Journal of Health, Population and Nutrition.2024;[Epub] CrossRef - Subchronic exposure to 1,2-naphthoquinone induces adipose tissue inflammation and changes the energy homeostasis of mice, partially due to TNFR1 and TLR4
Clílton Kraüss de Oliveira Ferreira, Clara Machado Campolim, Olívia Pizetta Zordão, Fernando Moreira Simabuco, Chadi Pellegrini Anaruma, Rodrigo Martins Pereira, Vitor Ferreira Boico, Luiz Guilherme Salvino, Maíra Maftoum Costa, Nathalia Quintero Ruiz, Le
Toxicology Reports.2023; 11: 10. CrossRef - Effects of Ambient Particulate Matter (PM2.5) Exposure on Calorie Intake and Appetite of Outdoor Workers
Thavin Kumar Mathana Sundram, Eugenie Sin Sing Tan, Hwee San Lim, Farahnaz Amini, Normina Ahmad Bustami, Pui Yee Tan, Navedur Rehman, Yu Bin Ho, Chung Keat Tan
Nutrients.2022; 14(22): 4858. CrossRef - Efficiency in reducing air pollutants and healthcare expenditure in the Seoul Metropolitan City of South Korea
Subal C. Kumbhakar, Jiyeon An, Masoomeh Rashidghalam, Almas Heshmati
Environmental Science and Pollution Research.2021; 28(20): 25442. CrossRef - Seasonal variation and trends in the Internet searches for losing weight: An infodemiological study
Ying Teng, Shun-Wei Huang, Zhen Li, Qiao-Mei Xie, Man Zhang, Qiu-Yue Lou, Fang Wang, Yan-Feng Zou
Obesity Research & Clinical Practice.2020; 14(3): 225. CrossRef - Estimation of health benefits from air quality improvement using the MODIS AOD dataset in Seoul, Korea
Daeun Kim, Jeongyeong Kim, Jaehwan Jeong, Minha Choi
Environmental Research.2019; 173: 452. CrossRef - Appropriate Medical Technology in the Era of the 4th Industrial Revolution
Sang Youl Rhee
The Korean Journal of Medicine.2019; 94(5): 387. CrossRef - Can Air Pollution Biologically Hinder Efforts to Lose Body Weight?
Duk-Hee Lee
Diabetes & Metabolism Journal.2018; 42(4): 282. CrossRef
- What could be the reasons for not losing weight even after following a weight loss program?
- Clinical Care/Education
- Diabetes Camp as Continuing Education for Diabetes Self-Management in Middle-Aged and Elderly People with Type 2 Diabetes Mellitus
- So Young Park, Sun Young Kim, Hye Mi Lee, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee, Kang-Hee Sim, Sang-Man Jin
- Diabetes Metab J. 2017;41(2):99-112. Published online March 3, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.2.99
- 4,180 View
- 43 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Despite the established benefits of diabetes camps for the continuing education of children with type 1 diabetes mellitus, little is known about the long-term metabolic benefits of diabetes camps for middle-aged and elderly people with type 2 diabetes mellitus (T2DM), especially in terms of glycosylated hemoglobin (HbA1c) variability.
Methods The 1-year mean and variability of HbA1c before and after the diabetes camp was compared between the participants of the diabetes camp (
n =57; median age 65 years [range, 50 to 86 years]; median diabetes duration 14 years [range, 1 to 48 years]). Additional case-control analysis compared the metabolic outcomes of the participants of the diabetes camp and their propensity score-matched controls who underwent conventional diabetes education (n =93).Results The levels of HbA1c during the first year after the diabetes camp were comparable to those of the matched controls (
P =0.341). In an analysis of all participants of the diabetes camp, the 1-year mean±standard deviation (SD) of HbA1c decreased (P =0.010 andP =0.041) after the diabetes camp, whereas the adjusted SD and coefficient of variance (CV) of HbA1c did not decrease. The adjusted SD and CV significantly decreased after the diabetes camp in participants whose 1-year mean HbA1c was ≥6.5% before the diabetes camp (n =40) and those with a duration of diabetes less than 15 years (n =32).Conclusion The 1-year mean and SD of HbA1c decreased after the diabetes camp, with significant reduction in the adjusted SD and CV in those with higher baseline HbA1c and a shorter duration of diabetes.
-
Citations
Citations to this article as recorded by- Older adults’ experiences of being at a senior summer camp—A phenomenographic study
Veronika Wallroth, Kjerstin Larsson, Agneta Schröder
Qualitative Social Work.2022; 21(5): 956. CrossRef - Pushing for miracles, pulling away from risk: An ethnographic analysis of the force dynamics at Senior Summer Camps in Sweden
Gabriella Nilsson, Lisa Ekstam, Janicke Andersson
Journal of Aging Studies.2018; 47: 96. CrossRef
- Older adults’ experiences of being at a senior summer camp—A phenomenographic study
- Response: Effects of Rebamipide on Gastrointestinal Symptoms in Patients with Type 2 Diabetes Mellitus (
Diabetes Metab J 2016;40:240-7) - Sejeong Park, So Young Park, Sang Youl Rhee
- Diabetes Metab J. 2016;40(4):336-337. Published online August 18, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.4.336
- 2,792 View
- 39 Download
- Others
- Effects of Rebamipide on Gastrointestinal Symptoms in Patients with Type 2 Diabetes Mellitus
- Sejeong Park, So Young Park, Yu Jin Kim, Soo Min Hong, Suk Chon, Seungjoon Oh, Jeong-taek Woo, Sung-Woon Kim, Young Seol Kim, Sang Youl Rhee
- Diabetes Metab J. 2016;40(3):240-247. Published online April 5, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.240
- 5,256 View
- 61 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Gastrointestinal (GI) symptoms are common in patients with type 2 diabetes mellitus (T2DM). Rebamipide is an effective gastric cytoprotective agent, but there are few data on its usefulness in T2DM. The aim of this study is to evaluate the improvement of GI symptoms after rebamipide treatment in patients with T2DM.
Methods Patients with T2DM and atypical GI symptoms were enrolled. They took rebamipide (100 mg thrice daily) for 12 weeks and filled out the diabetes bowel symptom questionnaire (DBSQ) before and after rebamipide treatment. The DBSQ consisted of 10 questions assessing the severity of GI symptoms by a 1 to 6 scoring system. Changes in the DBSQ scores before and after rebamipide treatment were analyzed to evaluate any improvements of GI symptoms.
Results A total of 107 patients were enrolled, and 84 patients completed the study. The mean age was 65.0±7.8, 26 patients were male (24.8%), the mean duration of T2DM was 14.71±9.12 years, and the mean glycosylated hemoglobin level was 6.97%±0.82%. The total DBSQ score was reduced significantly from 24.9±8.0 to 20.4±7.3 before and after rebamipide treatment (
P <0.001). The DBSQ scores associated with reflux symptoms, indigestion, nausea or vomiting, abdominal bloating or distension, peptic ulcer, abdominal pain, and constipation were improved after rebamipide treatment (P <0.05). However, there were no significant changes in symptoms associated with irritable bowel syndrome, diarrhea, and anal incontinence. No severe adverse events were reported throughout the study.Conclusion Rebamipide treatment for 12 weeks improved atypical GI symptoms in patients with T2DM.
-
Citations
Citations to this article as recorded by- Effectiveness of Rebamipide as a part of the Helicobacter pylori eradication therapy in Russia: a meta-analysis of controlled trials
Dmitry N. Andreev, Igor V. Maev, Dmitry S. Bordin, Svetlana V. Lyamina, Diana T. Dicheva, Aleksei K. Fomenko, Armine S. Bagdasarian
Consilium Medicum.2022; 24(5): 333. CrossRef - Сompliance in patients with coronary heart disease and erosive-ulcerative gastroduodenopathy
A. R. Molchanova, A. I. Dolgushina, A. A. Seljanina
Experimental and Clinical Gastroenterology.2020; (6): 82. CrossRef - Rebamipide: evidence base for use in gastroenterology
D. N. Andreev, I. V. Maev
Terapevticheskii arkhiv.2020; 92(12): 97. CrossRef - Efficacy of Rebamipide in Organic and Functional Dyspepsia: A Systematic Review and Meta-Analysis
Mohamed Hasif Jaafar, Sher Zaman Safi, Maw-Pin Tan, Sanjay Rampal, Sanjiv Mahadeva
Digestive Diseases and Sciences.2018; 63(5): 1250. CrossRef - Letter: Effects of Rebamipide on Gastrointestinal Symptoms in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2016;40:240-7)
Jin Hwa Kim
Diabetes & Metabolism Journal.2016; 40(4): 334. CrossRef - Response: Effects of Rebamipide on Gastrointestinal Symptoms in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2016;40:240-7)
Sejeong Park, So Young Park, Sang Youl Rhee
Diabetes & Metabolism Journal.2016; 40(4): 336. CrossRef
- Effectiveness of Rebamipide as a part of the Helicobacter pylori eradication therapy in Russia: a meta-analysis of controlled trials
- A Smartphone Application Significantly Improved Diabetes Self-Care Activities with High User Satisfaction
- Yu Jin Kim, Sang Youl Rhee, Jong Kyu Byun, So Young Park, Soo Min Hong, Sang Ouk Chin, Suk Chon, Seungjoon Oh, Jeong-taek Woo, Sung Woon Kim, Young Seol Kim
- Diabetes Metab J. 2015;39(3):207-217. Published online April 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.207
- 9,834 View
- 63 Download
- 37 Web of Science
- 48 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We developed for the first time a smartphone application designed for diabetes self-management in Korea and registered a patent for the relevant algorithm. We also investigated the user satisfaction with the application and the change in diabetes related self-care activities after using the application.
Methods We conducted a questionnaire survey on volunteers with diabetes who were using the application. Ninety subjects responded to the questionnaire between June 2012 and March 2013. A modified version of the Summary of Diabetes Self-Care Activities (SDSCA) was used in this study.
Results The survey results exhibited a mean subject age of 44.0 years old, and males accounted for 78.9% of the subjects. Fifty percent of the subjects had diabetes for less than 3 years. The majority of respondents experienced positive changes in their clinical course after using the application (83.1%) and were satisfied with the structure and completeness of the application (86.7%). Additionally, the respondents' answers indicated that the application was easy to use (96.7%) and recommendable to others (97.7%) and that they would continue using the application to manage their diabetes (96.7%). After using the Diabetes Notepad application, diabetes related self-care activities assessed by SDSCA displayed statistically significant improvements (
P <0.05), except for the number of days of drinking.Conclusion This smartphone-based application can be a useful tool leading to positive changes in diabetes related self-care activities and increase user satisfaction.
-
Citations
Citations to this article as recorded by- Time Efficiency, Reliability, and User Satisfaction of the Tooth Memo App for Recording Oral Health Information: Cross-Sectional Questionnaire Study
Palinee Detsomboonrat, Pagaporn Pantuwadee Pisarnturakit
JMIR Formative Research.2024; 8: e56143. CrossRef - Weight Management Health Note, a Mobile Health Platform for Obesity Management Developed by the Korean Society for the Study of Obesity
Yujung Lee, Hyunji Sang, Sunyoung Kim, Doo Ah Choi, Sang Youl Rhee
Journal of Obesity & Metabolic Syndrome.2024; 33(1): 1. CrossRef - Relationship between Diabetes Self-Management and the Use of Health Care Apps: A Cross-Sectional Study
Satoshi Inagaki, Kenji Kato, Kozue Abe, Hiroaki Takahashi, Tomokazu Matsuda
ACI Open.2023; 07(01): e23. CrossRef - The effect of mHealth program on behavior modification and health outcomes among patients with diabetes: A randomized controlled trial study
Mohd Khairul Zul Hasymi Firdaus, Piyanuch Jittanoon, Umaporn Boonyasopun, Muhammad Kamil Che Hasan
Belitung Nursing Journal.2023; 9(5): 437. CrossRef - Clinical Effects of a Home Care Pilot Program for Patients with Type 1 Diabetes Mellitus: A Retrospective Cohort Study
Sejeong Lee, KyungYi Kim, Ji Eun Kim, Yura Hyun, Minyoung Lee, Myung-Il Hahm, Sang Gyu Lee, Eun Seok Kang
Diabetes & Metabolism Journal.2023; 47(5): 693. CrossRef - Mobile-Based Application Interventions to Enhance Cancer Control and Care in Low- and Middle-Income Countries: A Systematic Review
Andrew Donkor, Jennifer Akyen Ayitey, Prince Nyansah Adotey, Esther Oparebea Ofori, Doris Kitson-Mills, Verna Vanderpuye, Samuel Yaw Opoku, Tim Luckett, Meera R. Agar, Penelope Engel-Hills
International Journal of Public Health.2023;[Epub] CrossRef - Effect of an Integrative Mobile Health Intervention in Patients With Hypertension and Diabetes: Crossover Study
Sang Woo Oh, Kyoung-Kon Kim, Sung Soo Kim, Su Kyung Park, Sangshin Park
JMIR mHealth and uHealth.2022; 10(1): e27192. CrossRef - Evaluation of a Smart After-Care Program for Patients with Lung Cancer: A Prospective, Single-Arm Pilot Study
Hee Chul Yang, Seung Hyun Chung, Ji Sung Yoo, Boram Park, Moon Soo Kim, Jong Mog Lee
Journal of Chest Surgery.2022; 55(2): 108. CrossRef - Personalized Nutrition for the Prevention and Treatment of Metabolic Diseases: Opportunities and Perspectives
I. N. Napolsky, P. V. Popova
Russian Journal for Personalized Medicine.2022; 2(1): 15. CrossRef - The effect of a mobile application on the foot care of individuals with type 2 diabetes: A randomised controlled study
Berna Dincer, Nefise Bahçecik
Health Education Journal.2021; 80(4): 425. CrossRef - Effectiveness of Disease-Specific mHealth Apps in Patients With Diabetes Mellitus: Scoping Review
Claudia Eberle, Maxine Löhnert, Stefanie Stichling
JMIR mHealth and uHealth.2021; 9(2): e23477. CrossRef - Diabetology 4.0: Scoping Review of Novel Insights and Possibilities Offered by Digitalization
Claudia Eberle, Stefanie Stichling, Maxine Löhnert
Journal of Medical Internet Research.2021; 23(3): e23475. CrossRef - Mobile Healthcare System Provided by Primary Care Physicians Improves Quality of Diabetes Care
Tae Jung Oh, Jie-Eun Lee, Seok Kim, Sooyoung Yoo, Hak Chul Jang
CardioMetabolic Syndrome Journal.2021; 1(1): 88. CrossRef - A Personalized Mobile Health Program for Type 2 Diabetes During the COVID-19 Pandemic: Single-Group Pre–Post Study
Ian Yi Han Ang, Kyle Xin Quan Tan, Clive Tan, Chiew Hoon Tan, James Wei Ming Kwek, Joanne Tay, Sue Anne Toh
JMIR Diabetes.2021; 6(3): e25820. CrossRef - The use of mobile health interventions for gestational diabetes mellitus: a descriptive literature review
Maryam Zahmatkeshan, Somayyeh Zakerabasali, Mojtaba Farjam, Yousef Gholampour, Maryam Seraji, Azita Yazdani
Journal of Medicine and Life.2021; 14(2): 131. CrossRef - Methods and Measures Used to Evaluate Patient-Operated Mobile Health Interventions: Scoping Literature Review
Meghan Bradway, Elia Gabarron, Monika Johansen, Paolo Zanaboni, Patricia Jardim, Ragnar Joakimsen, Louise Pape-Haugaard, Eirik Årsand
JMIR mHealth and uHealth.2020; 8(4): e16814. CrossRef - Effect of a Mobile Phone–Based Glucose-Monitoring and Feedback System for Type 2 Diabetes Management in Multiple Primary Care Clinic Settings: Cluster Randomized Controlled Trial
Yeoree Yang, Eun Young Lee, Hun-Sung Kim, Seung-Hwan Lee, Kun-Ho Yoon, Jae-Hyoung Cho
JMIR mHealth and uHealth.2020; 8(2): e16266. CrossRef - Methods and Evaluation Criteria for Apps and Digital Interventions for Diabetes Self-Management: Systematic Review
Dillys Larbi, Pietro Randine, Eirik Årsand, Konstantinos Antypas, Meghan Bradway, Elia Gabarron
Journal of Medical Internet Research.2020; 22(7): e18480. CrossRef - Evaluating the effect of a smartphone app-based self-management program for people with COPD: A randomized controlled trial
Soo Kyung Park, Cho Hee Bang, Seung Hyeun Lee
Applied Nursing Research.2020; 52: 151231. CrossRef - Development of an mHealth application for family carers of people with dementia: A study protocol
Sarath Rathnayake, Wendy Moyle, Cindy Jingwen Jones, Pauline Calleja
Collegian.2019; 26(2): 295. CrossRef - Use of Weight-Management Mobile Phone Apps in Saudi Arabia: A Web-Based Survey
Ghadeer S Aljuraiban
JMIR mHealth and uHealth.2019; 7(2): e12692. CrossRef - Appropriate Medical Technology in the Era of the 4th Industrial Revolution
Sang Youl Rhee
The Korean Journal of Medicine.2019; 94(5): 387. CrossRef - Popular Diabetes Apps and the Impact of Diabetes App Use on Self-Care Behaviour: A Survey Among the Digital Community of Persons With Diabetes on Social Media
Mihiretu M. Kebede, Claudia R. Pischke
Frontiers in Endocrinology.2019;[Epub] CrossRef - Development and Evaluation: The Satisfaction of Using an Oral Health Survey Mobile Application
Palinee Detsomboonrat, Pagaporn Pantuwadee Pisarnturakit
Telemedicine and e-Health.2019; 25(1): 55. CrossRef - Usability of a Disease Management Mobile Application as Perceived by Patients With Diabetes
Roqaieh Janatkhah, Rasoul Tabari-Khomeiran, Attaolah Asadi-Louyeh, Ehsan Kazemnejad
CIN: Computers, Informatics, Nursing.2019; 37(8): 413. CrossRef - Structure and Characteristics of Diabetes Self-management Applications
Sara Angelini, Gregorio Marco Alicastro, Sara Dionisi, Marco Di Muzio
CIN: Computers, Informatics, Nursing.2019; 37(7): 340. CrossRef - Digital Health Transformation of Integrated Care in Europe: Overarching Analysis of 17 Integrated Care Programs
Erik Baltaxe, Thomas Czypionka, Markus Kraus, Miriam Reiss, Jan Erik Askildsen, Renata Grenkovic, Tord Skogedal Lindén, János György Pitter, Maureen Rutten-van Molken, Oscar Solans, Jonathan Stokes, Verena Struckmann, Josep Roca, Isaac Cano
Journal of Medical Internet Research.2019; 21(9): e14956. CrossRef - A Mobile Prenatal Care App to Reduce In-Person Visits: Prospective Controlled Trial
Kathryn I Marko, Nihar Ganju, Jill M Krapf, Nancy D Gaba, James A Brown, Joshua J Benham, Julia Oh, Lorna M Richards, Andrew C Meltzer
JMIR mHealth and uHealth.2019; 7(5): e10520. CrossRef - Users’ preferences and design recommendations to promote engagements with mobile apps for diabetes self-management: Multi-national perspectives
Mary D. Adu, Usman H. Malabu, Aduli E. O. Malau-Aduli, Bunmi S. Malau-Aduli, Simone Borsci
PLOS ONE.2018; 13(12): e0208942. CrossRef - Developing and Clinical Application of a Smartphone Mobile Mood Chart Application in Korean for Patients with Bipolar Disorder
Kayoung Song, Saejeong Lee, Woon Yoon, Changyoon Kim, Yeonho Joo, Jungsun Lee, Myong-Wuk Chon
Journal of Korean Neuropsychiatric Association.2018; 57(3): 244. CrossRef - mHealth Tools for the Self-Management of Patients With Multimorbidity in Primary Care Settings: Pilot Study to Explore User Experience
Anum Irfan Khan, Ashlinder Gill, Cheryl Cott, Parminder Kaur Hans, Carolyn Steele Gray
JMIR mHealth and uHealth.2018; 6(8): e171. CrossRef - Rules of engagement in mobile health: what does mobile health bring to research and theory?
Cigdem Sahin
Contemporary Nurse.2018; 54(4-5): 374. CrossRef - Diabetes Mellitus m-Health Applications: A Systematic Review of Features and Fundamentals
Ericles Andrei Bellei, Daiana Biduski, Nathália Pinto Cechetti, Ana Carolina Bertoletti De Marchi
Telemedicine and e-Health.2018; 24(11): 839. CrossRef - Current Status and Effects of Nutrition Education Programs for Diabetic Patients in Korea
Hae Jin Kang
The Journal of Korean Diabetes.2018; 19(2): 106. CrossRef - Mobile direct observation of therapy (MDOT) - A rapid systematic review and pilot study in children with asthma
Michael D. Shields, Fahad ALQahtani, Michael P. Rivey, James C. McElnay, Jacobus P. van Wouwe
PLOS ONE.2018; 13(2): e0190031. CrossRef - App-basiertes Selbstmonitoring bei Typ-2-Diabetes
A. Steinert, M. Haesner, E. Steinhagen-Thiessen
Zeitschrift für Gerontologie und Geriatrie.2017; 50(6): 516. CrossRef - Smartphone App Use for Diabetes Management: Evaluating Patient Perspectives
Kirstie Lithgow, Alun Edwards, Doreen Rabi
JMIR Diabetes.2017; 2(1): e2. CrossRef - Needs for Development of IT-based Nutritional Management Program for Women with Gestational Diabetes Mellitus
Chan-Jung Han, Sun-Young Lim, Eunsuk Oh, Yoon-Hee Choi, Kun-Ho Yoon, Jin-Hee Lee
Korean Journal of Community Nutrition.2017; 22(3): 207. CrossRef - Semantic representation and processing of hypoglycemic events derived from wearable sensor data
Jean-Paul Calbimonte, Jean-Eudes Ranvier, Fabien Dubosson, Karl Aberer, Antonis Bikakis, Thanos G. Stavropoulos, Georgios Meditskos
Journal of Ambient Intelligence and Smart Environments.2017; 9(1): 97. CrossRef - Acceptability and Feasibility of a Smartphone Application for 5th, 6th Grade Elementary Students to Prevent Childhood Obesity; a Qualitative Study
Ji-Hye Jung, Young-Gyu Cho, Da-Ye Ji, Jae-Heon Kang
Korean Journal of Health Promotion.2016; 16(4): 251. CrossRef - m-santé francophone et diabète : mise au point
M. Halbron, M. Joubert, E. Sonnet
Médecine des Maladies Métaboliques.2016; 10(3): 243. CrossRef - Successful weight reduction and maintenance by using a smartphone application in those with overweight and obesity
Sang Ouk Chin, Changwon Keum, Junghoon Woo, Jehwan Park, Hyung Jin Choi, Jeong-taek Woo, Sang Youl Rhee
Scientific Reports.2016;[Epub] CrossRef - The Wills Eye Glaucoma App: Interest of Patients and Their Caregivers in a Smartphone-based and Tablet-based Glaucoma Application
Michael Waisbourd, Hermandeep Dhami, Chen Zhou, Michael Hsieh, Pramod Abichandani, Michael J. Pro, Marlene R. Moster, L. Jay Katz, Lisa A. Hark, Jonathan S. Myers
Journal of Glaucoma.2016; 25(9): e787. CrossRef - Testing the Feasibility of Remote Patient Monitoring in Prenatal Care Using a Mobile App and Connected Devices: A Prospective Observational Trial
Kathryn I Marko, Jill M Krapf, Andrew C Meltzer, Julia Oh, Nihar Ganju, Anjali G Martinez, Sheetal G Sheth, Nancy D Gaba
JMIR Research Protocols.2016; 5(4): e200. CrossRef - Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef - Efficacy of a New Medical Information system, Ubiquitous Healthcare Service with Voice Inception Technique in Elderly Diabetic Patients
Kyoung Min Kim, Kyeong Seon Park, Hyun Ju Lee, Yun Hee Lee, Ji Seon Bae, Young Joon Lee, Sung Hee Choi, Hak Chul Jang, Soo Lim
Scientific Reports.2015;[Epub] CrossRef - Six-month Outcomes of Mobile Phone Application-based Self-management in a Patient with Type 2 Diabetes
Mi Kyeong Hong, Young Yun Cho, Mi Yong Rha, Jae Hyeon Kim, Moon-Kyu Lee
Clinical Nutrition Research.2015; 4(3): 201. CrossRef - Physical Activity Capture Technology With Potential for Incorporation Into Closed-Loop Control for Type 1 Diabetes
Vikash Dadlani, James A. Levine, Shelly K. McCrady-Spitzer, Eyal Dassau, Yogish C. Kudva
Journal of Diabetes Science and Technology.2015; 9(6): 1208. CrossRef
- Time Efficiency, Reliability, and User Satisfaction of the Tooth Memo App for Recording Oral Health Information: Cross-Sectional Questionnaire Study
- Intracerebroventricular Injection of Metformin Induces Anorexia in Rats
- Chang Koo Lee, Yoon Jung Choi, So Young Park, Jong Yeon Kim, Kyu Chang Won, Yong Woon Kim
- Diabetes Metab J. 2012;36(4):293-299. Published online August 20, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.4.293
- 4,447 View
- 42 Download
- 27 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Metformin, an oral biguanide insulin-sensitizing agent, is well known to decrease appetite. Although there is evidence that metformin could affect the brain directly, the exact mechanism is not yet known.
Methods To evaluate whether metformin induces anorexia via the hypothalamus, various concentrations of metformin were injected into the lateral ventricle of rats through a chronically implanted catheter and food intake was measured for 24 hours. The hypothalamic neuropeptides associated with regulation of food intake were also analyzed following 1 hour of intracerebroventricular (ICV) injections of metformin.
Results An ICV injection of metformin decreased food intake in a dose-dependent manner in unrestrained conscious rats. Hypothalamic phosphorylated AMP-activated protein kinase (pAMPK) increased by 3 µg with metformin treatment, but there was no further increase in pAMPK with increases in metformin dosage. The hypothalamic phosphorylated signal transducer and activator of transcription 3 (pSTAT3) increased by 3 µg with metformin treatment, but, there was no further increase in pSTAT3 level following increases of metformin dosage. Hypothalamic proopiomelanocortin was elevated with metformin treatment, while neuropeptide Y was not significantly changed.
Conclusion Our results suggest that metformin induces anorexia via direct action in the hypothalamus and the increase in pSTAT3, at least in part, is involved in the process. However, hypothalamic pAMPK appears not to contribute to metformin-induced appetite reduction in normal rats. Further studies exploring new pathways connecting metformin and feeding regulation are needed.
-
Citations
Citations to this article as recorded by- Metabolic and Metabolomic Effects of Metformin in Murine Model of Pulmonary Adenoma Formation
Andrew C. Elton, Vannesa Cedarstrom, Arman Quraishi, Beverly Wuertz, Kevin Murray, Todd W. Markowski, Donna Seabloom, Frank G. Ondrey
Nutrition and Cancer.2023; 75(3): 1014. CrossRef - Steroidogenic Effect of Luteinizing Hormone Receptor Agonists and Metformin in Male Rats with Androgenic Deficiency Caused by Diet-Induced Obesity
A. A. Bakhtyukov, K. V. Derkach, I. A. Lebedev, V. N. Sorokoumov, A. O. Shpakov
Journal of Evolutionary Biochemistry and Physiology.2023; 59(5): 1810. CrossRef - Steroidogenic Effect of Luteinizing Hormone Receptor Agonists and Metformin in Male Rats with Androgenic Deficiency Caused by Diet-Induced Obesity
A. A. Bakhtyukov, K. V. Derkach, I. A. Lebedev, V. N. Sorokoumov, A. O. Shpakov
Российский физиологический журнал им И М Сеченова.2023; 109(10): 1414. CrossRef - Metformin in nucleus accumbens core reduces cue‐induced cocaine seeking in male and female rats
Amy Chan, Alexis Willard, Sarah Mulloy, Noor Ibrahim, Allegra Sciaccotta, Mark Schonfeld, Sade M. Spencer
Addiction Biology.2022;[Epub] CrossRef - Knockdown of Endogenous Nucb2/Nesfatin-1 in the PVN Leads to
Obese-Like Phenotype and Abolishes the Metformin- and Stress-Induced Thermogenic
Response in Rats
Daniel Stephan, Natalie Taege, Riccardo Dore, Julica Folberth, Olaf Jöhren, Markus Schwaninger, Hendrik Lehnert, Carla Schulz
Hormone and Metabolic Research.2022; 54(11): 768. CrossRef - Modulation of hypothalamic AMPK phosphorylation by olanzapine controls energy balance and body weight
Vitor Ferreira, Cintia Folgueira, Maria Guillén, Pablo Zubiaur, Marcos Navares, Assel Sarsenbayeva, Pilar López-Larrubia, Jan W. Eriksson, Maria J. Pereira, Francisco Abad-Santos, Guadalupe Sabio, Patricia Rada, Ángela M. Valverde
Metabolism.2022; 137: 155335. CrossRef - Metformin acts on the gut-brain axis to ameliorate antipsychotic-induced metabolic dysfunction
Xiaorong Wang, Huimin Huang, Yiyi Zhu, Shaoli Li, Peifen Zhang, Jiajun Jiang, Caixi Xi, Lingling Wu, Xingle Gao, Yaoyang Fu, Danhua Zhang, Yiqing Chen, Shaohua Hu, Jianbo Lai
BioScience Trends.2021; 15(5): 321. CrossRef - Therapeutic effect of treatment with metformin and/or 4-hydroxychalcone in male Wistar rats with nonalcoholic fatty liver disease
Selene de Jesús Acosta-Cota, Elsa Maribel Aguilar-Medina, Rosalío Ramos-Payán, José Guadalupe Rendón Maldonado, José Geovanni Romero-Quintana, Julio Montes-Avila, Juan I. Sarmiento-Sánchez, Carolina Gabriela Plazas-Guerrero, Marcela J. Vergara-Jiménez, Ar
European Journal of Pharmacology.2019; 863: 172699. CrossRef - The evidence of metabolic-improving effect of metformin in Ay/a mice with genetically-induced melanocortin obesity and the contribution of hypothalamic mechanisms to this effect
Kira Derkach, Irina Zakharova, Inna Zorina, Andrey Bakhtyukov, Irina Romanova, Liubov Bayunova, Alexander Shpakov, Guillermo López Lluch
PLOS ONE.2019; 14(3): e0213779. CrossRef - Effect of Metformin on Antipsychotic-Induced Metabolic Dysfunction: The Potential Role of Gut-Brain Axis
Chao Luo, Xu Wang, Hanxue Huang, Xiaoyuan Mao, Honghao Zhou, Zhaoqian Liu
Frontiers in Pharmacology.2019;[Epub] CrossRef - Metformin alters signaling induced crosstalk and homeostasis in the carcinogenesis paradigm “Epistemology of the origin of cancer”
Björn L.D.M. Brücher, Ijaz S. Jamall, Obul R. Bandapalli
4open.2019; 2: 12. CrossRef - Melatonin potentiates the effects of metformin on glucose metabolism and food intake in high‐fat‐fed rats
Rosana F. Dantas‐Ferreira, Helene Raingard, Stephanie Dumont, Carole Schuster‐Klein, Beatrice Guardiola‐Lemaitre, Paul Pevet, Etienne Challet
Endocrinology, Diabetes & Metabolism.2018;[Epub] CrossRef -
Molecular Mechanisms of the Effects of Metformin on the Functional Activity of Brain Neurons
A. O. Shpakov, K. V. Derkach
Neuroscience and Behavioral Physiology.2018; 48(8): 969. CrossRef - Effect of metformin/irinotecan-loaded poly-lactic-co-glycolic acid nanoparticles on glioblastoma: in vitro and in vivo studies
Ali Taghizadehghalehjoughi, Ahmet Hacimuftuoglu, Meltem Cetin, Afife Busra Ugur, Bianca Galateanu, Yaroslav Mezhuev, Ufuk Okkay, Numan Taspinar, Mehmet Taspinar, Abdullah Uyanik, Betul Gundogdu, Maryam Mohammadzadeh, Kemal Alp Nalci, Polychronis Stivaktak
Nanomedicine.2018; 13(13): 1595. CrossRef - Effect of Betahistine and Metformin on Antipsychotic-Induced Weight Gain: An Analysis of Two Clinical Trials
Dongyu Kang, Zhihui Jing, Ranran Li, Gangrui Hei, Tiannan Shao, Li Li, Mengxi Sun, Ye Yang, Ying Wang, Xiaoyi Wang, Yujun Long, Xiansheng Huang, Renrong Wu
Frontiers in Psychiatry.2018;[Epub] CrossRef - Metformin: not only per os
Lev M. Berstein
Expert Review of Endocrinology & Metabolism.2018; 13(2): 63. CrossRef - МЕТАБОЛИЧЕСКИЕ ПОКАЗАТЕЛИ И ФУНКЦИОНАЛЬНОЕ СОСТОЯНИЕ СИГНАЛЬНЫХ СИСТЕМ ГИПОТАЛАМУСА И ВЛИЯНИЕ НА НИХ МЕТФОРМИНА У МЫШЕЙ С МУТАЦИЕЙ AY/A, ГЕНЕТИЧЕСКИ ПРЕДРАСПОЛОЖЕННЫХ К ОЖИРЕНИЮ, "Доклады Академии наук"
К.В. Деркач, И.О. Захарова, И.В. Романова, И. И. Зорина, А.Л. Михрина, А.О. Шпаков
Доклады Академии Наук.2017; (4): 488. CrossRef - Beneficial effects of metformin on energy metabolism and visceral fat volume through a possible mechanism of fatty acid oxidation in human subjects and rats
Ichiro Tokubuchi, Yuji Tajiri, Shimpei Iwata, Kento Hara, Nobuhiko Wada, Toshihiko Hashinaga, Hitomi Nakayama, Hiroharu Mifune, Kentaro Yamada, M. Faadiel Essop
PLOS ONE.2017; 12(2): e0171293. CrossRef - Metabolic parameters and functional state of hypothalamic signaling systems in AY/a mice with genetic predisposition to obesity and the effect of metformin
K. V. Derkach, I. O. Zakharova, I. V. Romanova, I. I. Zorina, A. L. Mikhrina, A. O. Shpakov
Doklady Biochemistry and Biophysics.2017; 477(1): 377. CrossRef - Prolonged metformin treatment leads to reduced transcription of Nrf2 and neurotrophic factors without cognitive impairment in older C57BL/6J mice
Joanne S. Allard, Evelyn J. Perez, Koji Fukui, Priscilla Carpenter, Donald K. Ingram, Rafael de Cabo
Behavioural Brain Research.2016; 301: 1. CrossRef - Intracerebroventricular Metformin Decreases Body Weight But Has Pro-oxidant Effects and Decreases Survival
Luis Valmor Portela, Jussania Gnoatto, Andressa Wigner Brochier, Clarissa Branco Haas, Adriano Martimbianco de Assis, Afonso Kopczynski de Carvalho, Gisele Hansel, Eduardo Rigon Zimmer, Jean Pierre Oses, Alexandre Pastoris Muller
Neurochemical Research.2015; 40(3): 514. CrossRef - Metformin alleviates hepatosteatosis by restoring SIRT1-mediated autophagy induction via an AMP-activated protein kinase-independent pathway
Young Mi Song, Yong-ho Lee, Ji-Won Kim, Dong-Sik Ham, Eun-Seok Kang, Bong Soo Cha, Hyun Chul Lee, Byung-Wan Lee
Autophagy.2015; 11(1): 46. CrossRef - Activation of AMP-activated protein kinase by metformin protects against global cerebral ischemia in male rats: Interference of AMPK/PGC-1α pathway
Ghorbangol Ashabi, Fariba Khodagholi, Leila Khalaj, Mahdi Goudarzvand, Masoumeh Nasiri
Metabolic Brain Disease.2014; 29(1): 47. CrossRef - Acute oral metformin enhances satiation and activates brainstem nesfatinergic neurons
Thaïs Rouquet, Pierre Clément, Stéphanie Gaigé, Catherine Tardivel, Julien Roux, Michel Dallaporta, Bruno Bariohay, Jean-Denis Troadec, Bruno Lebrun
Obesity.2014; : n/a. CrossRef - Metformin—mode of action and clinical implications for diabetes and cancer
Ida Pernicova, Márta Korbonits
Nature Reviews Endocrinology.2014; 10(3): 143. CrossRef - Effects of metformin on weight loss
Steven K. Malin, Sangeeta R. Kashyap
Current Opinion in Endocrinology, Diabetes & Obesity.2014; 21(5): 323. CrossRef - The effect of ghrelin on MK-801 induced memory impairment in rats
Fatemeh Goshadrou, Mojtaba Kermani, Abdolaziz Ronaghi, Samad Sajjadi
Peptides.2013; 44: 60. CrossRef
- Metabolic and Metabolomic Effects of Metformin in Murine Model of Pulmonary Adenoma Formation

 KDA
KDA
 First
First Prev
Prev





